Introduction
Diabetes is a disease characterized by a relative or absolute lack of insulin, leading to hyperglycemia. There are two main types of diabetes: type 1 diabetes and type 2 diabetes. Type 1 diabetes is due to the autoimmune destruction of the insulin-producing pancreatic beta cells, and type 2 diabetes is caused by insulin resistance coupled with a failure of the beta cell to compensate. Animal models in diabetes research for type 1 diabetes range from animals with spontaneously developing autoimmune diabetes to chemical ablation of the pancreatic beta cells. Type 2 diabetes is modeled in both obese and non-obese animal models with varying degrees of insulin resistance and beta-cell failure. Diabetes Animal Testing
Diabetes mellitus is a chronic disease that is characterized by a relative or absolute lack of insulin, resulting in hyperglycaemia. Chronic hyperglycaemia can lead to a variety of complications such as neuropathy, nephropathy and retinopathy and increased risk of cardiovascular disease. Recent figures suggest the worldwide prevalence of diabetes is 9.2% in women and 9.8% in men, with approximately 347 million people suffering from the disease worldwide in 2008 (Danaei et al., 2011). There are several different classifications of diabetes, the most common being type 1 and type 2 diabetes.
Type 1 diabetes is an autoimmune disease leading to the destruction of the insulin-producing pancreatic beta cells in the islets of Langerhans. Type 1 diabetes is most commonly diagnosed in children and young adults, and by the time of diagnosis, patients have very little endogenous insulin production. Insulin therefore has to be replaced by regular subcutaneous injections, and blood glucose levels must be frequently monitored to manage the risk of hypoglycaemia.
Type 2 diabetes is the most common type of diabetes with prevalence in the United Kingdom of around 4%. It is most commonly diagnosed in middle-aged adults, although more recently the age of onset is decreasing with increasing levels of obesity (Pinhas-Hamiel and Zeitler, 2005). Indeed, although development of the disease shows high hereditability, the risk increases proportionally with body mass index (Lehtovirta et al., 2010). Type 2 diabetes is associated with insulin resistance, and a lack of appropriate compensation by the beta cells leads to a relative insulin deficiency. Insulin resistance can be improved by weight reduction and exercise (Solomon et al., 2008).
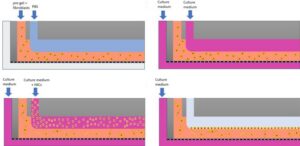
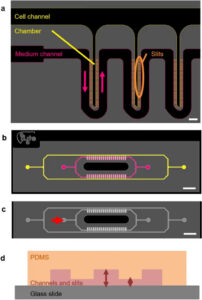
How to culture vascularized & immunocompetent 3D models in a standard Multiwell
Chemically induced type 1 diabetes
In chemically induced models of type 1 diabetes, a high percentage of the endogenous beta cells are destroyed, and thus, there is little endogenous insulin production, leading to hyperglycaemia and weight loss. Chemically induced diabetes not only provides a simple and relatively cheap model of diabetes in rodents but can also be used in higher animals (Dufrane et al., 2006). Diabetes Animal Testing
Spontaneous autoimmune animal models in diabetes research
The most commonly used autoimmune models of type 1 diabetes are the non-obese diabetic (NOD) mouse and the Biobreeding (BB) rat (Yang and Santamaria, 2006). In addition, another rat model of autoimmune type 1 the LEW.1AR1/Ztm-iddm rat was described in 2001 (Lenzen et al., 2001). However, the NOD mouse still dominates the literature as the autoimmune model of choice. Diabetes Animal Testing
Genetically induced insulin-dependent diabetes
The AKITA mouse was derived in Akita, Japan from a C57BL/6NSlc mouse with a spontaneous mutation in the insulin 2 gene preventing correct processing of pro-insulin. This causes an overload of misfolded proteins and subsequent ER stress. This results in a severe insulin-dependent diabetes starting from 3 to 4 weeks of age, which is characterized by hyperglycaemia, hypoinsulinaemia, polyuria and polydipsia. Untreated homozygotes rarely survive longer than 12 weeks. The lack of beta cell mass in this model makes it an alternative to streptozotocin-treated mice in transplantation studies (Mathews et al., 2002).

Virus-induced models of diabetes
Viruses have been implicated in the pathogenesis of type 1 diabetes (van der Werf et al., 2007). Therefore, several animal models have used viruses to initiate beta cell destruction. The destruction can be either due to direct infection of the beta cell or initiation of an autoimmune response against the beta cell (Jun and Yoon, 2003). Viruses used to induce diabetes in animal models include coxsackie B virus (Yoon et al., 1986; Kang et al., 1994; Jaidane et al., 2009), encephalomyocarditis virus (Craighead and McLane, 1968; Baek and Yoon, 1991; Shimada and Maruyama, 2004) and Kilham rat virus (Guberski et al., 1991; Ellerman et al., 1996).
Non-rodent models of type 1 diabetes
In addition to the extensively studied rodent models of type 1 diabetes, several large animal models have been developed. In large animal models, spontaneous diabetes is relatively rare and unpredictable in onset, and thus, induced models of type 1 diabetes are required. The most common method of inducing insulin dependence in large models is either by pancreatectomy or STZ.
Animal models of type 2 diabetes
Type 2 diabetes is characterized by insulin resistance and the inability of the beta cell to sufficiently compensate. Therefore, animal models of type 2 diabetes tend to include models of insulin resistance and/or models of beta cell failure. Many animal models of type 2 diabetes are obese, reflecting the human condition where obesity is closely linked to type 2 diabetes development. Some of the most commonly used models for type 2 diabetes are outlined in Table 2.
Obese models of type 2 diabetes
As type 2 diabetes is closely linked to obesity, most of the current animal models of type 2 diabetes are obese. Obesity can be the result of naturally occurring mutations or genetic manipulation. Alternatively, obesity can be induced by high fat feeding. Diabetes Animal Testing
High fat feeding
The model of high-fat feeding to C57BL/6 mice was first described in 1988 (Surwit et al., 1988). High fat feeding can lead to obesity, hyperinsulinemia and altered glucose homeostasis due to insufficient compensation by the islets (Winzell and Ahren, 2004). Normal chow (on a caloric basis usually around 26% protein, 63% carbohydrate, and 11% fat) is exchanged for a diet where the number of calories from fat is increased substantially (around 58% of energy derived from fat). The amount of food eaten should be monitored to ensure that the mice do not compensate by eating less. It has been shown that high-fat-fed mice can weigh more than chow-fed controls within a week of starting the high-fat diet (Winzell and Ahren, 2004), although typically mice are fed the high-fat diet for several weeks to induce a more pronounced weight gain. The weight gain is associated with insulin resistance, and lack of beta-cell compensation leads to impaired glucose tolerance. Diabetes Animal Testing
Nonobese models of type 2 diabetes
Not all type 2 diabetes patients are obese, and thus, it is important that lean animal models of type 2 diabetes are also studied. These include models that have beta cell inadequacy, which is what ultimately leads to overt type 2 diabetes in humans (Weir et al., 2009). Diabetes Animal Testing
Non-rodent models of type 2 diabetes
Larger animals have also been utilized in type 2 diabetes research. Type 2 diabetes in cats resembles the human condition in several aspects, including clinical, physiological and pathological aspects. Some characteristics common to humans include that type 2 diabetes in cats develops in middle age, is associated with obesity and insulin resistance, and subsequent beta cell loss occurs (O’Brien, 2002)
A variety of animal models of type 1 and type 2 diabetes are described above, each with their own characteristics. There are several different purposes that these models of diabetes could be used for including pharmacological testing, studies of genetics and understanding disease mechanisms. The choice of model will depend on the purpose of the study. For example, in the case of pharmacological testing, the putative mechanism of the drug being tested will be instrumental in choosing an appropriate animal model.
In type 1 diabetes, the main determinant in choosing an animal model is whether a model of autoimmunity is required. The timing and predictability of onset is also variable in different models of type 1 diabetes.
In type 2 diabetes, it is important to consider the mechanisms underlying the hyperglycaemia and whether this is relevant to your study. These mechanisms can include insulin resistance and/or beta cell failure. Indeed, to determine whether a drug intervention can improve symptoms in any given model may depend on whether beta cells have failed. Animal models of type 2 diabetes can be divided into those that are obese and those that are nonobese. The majority of type 2 diabetes models are obese, by either genetic or dietary means. However, this usually comes with a variety of associated pathologies such as dyslipidaemia and artherosclerosis. Although these co-morbidities are common in some humans with type 2 diabetes, it only represents a portion of the diabetic population.
References
The use of animal models in diabetes research – Aileen JF King
FAQ
Diabetes mellitus is known as a chronic disease. It is characterised by a relative or absolute lack of insulin, which results in hyperglycaemia. A variety of complications, such as neuropathy, nephropathy, and retinopathy, can be led to by chronic hyperglycaemia. The risk of cardiovascular disease is also increased. There are several different classifications of the disease. The most common types are Type 1 and Type 2 diabetes. Recent figures suggested a high worldwide prevalence of the disease. Approximately 347 million people were estimated to be suffering from diabetes worldwide in 2008\.
Type 1 diabetes is classified as an autoimmune disease. The destruction of the insulin-producing pancreatic beta cells is caused by this condition. These cells are located in the islets of Langerhans. This type of diabetes is most commonly diagnosed in children and young adults. By the time a diagnosis is made, patients are found to have very little endogenous insulin production. Insulin must be replaced. This is done by regular subcutaneous injections. Blood glucose levels also have to be monitored frequently. This monitoring is done to manage the risk of hypoglycaemia.
Type 2 diabetes is the most common type of the disease. A prevalence of around 4% in the United Kingdom is reported. It is most commonly diagnosed in middle-aged adults. The age of onset has been decreasing more recently. This decrease is associated with increasing levels of obesity. The disease shows high hereditability. The risk for developing it increases proportionally with body mass index. Type 2 diabetes is associated with insulin resistance. A lack of appropriate compensation by the beta cells leads to a relative insulin deficiency. Weight reduction and exercise can improve insulin resistance.
In chemically induced models of Type 1 diabetes, a high percentage of the endogenous beta cells is destroyed. Very little endogenous insulin production is left as a result. This lack of insulin leads to hyperglycaemia and weight loss. This method of chemically induced diabetes is considered a simple and relatively cheap model of the disease in rodents. It is not limited to rodents. The method can also be used in higher animals. One common method is the use of STZ (streptozotocin). This chemical is toxic to the beta cells and is also used to induce diabetes in large animal models.
Research into Type 1 diabetes can involve models of autoimmunity. The non-obese diabetic (NOD) mouse is the most commonly used autoimmune model. The Biobreeding (BB) rat is also used. Another rat model, the LEW.1AR1/Ztm-iddm rat, was described in 2001\. Despite the availability of these other models, the NOD mouse is still the dominant choice in the literature for an autoimmune model. These models are distinct from chemically induced models. They develop autoimmune diabetes spontaneously. This is more similar to the autoimmune destruction of beta cells that occurs in human Type 1 diabetes.
The AKITA mouse is a model of genetically induced insulin-dependent diabetes. It was derived in Japan from a C57BL/6NSlc mouse. This mouse line has a spontaneous mutation in the insulin 2 gene. The correct processing of pro-insulin is prevented by this mutation. An overload of misfolded proteins is caused, which leads to subsequent ER stress. A severe insulin-dependent diabetes is resulted, starting from 3 to 4 weeks of age. This condition is characterised by hyperglycaemia, hypoinsulinaemia, polyuria, and polydipsia. Untreated homozygotes rarely survive longer than 12 weeks. The lack of beta cell mass in this model makes it an alternative for transplantation studies.
In addition to rodent models, several large animal models have been developed for Type 1 diabetes research. Spontaneous diabetes in large animal models is relatively rare. Its onset is also unpredictable. Because of this, induced models of Type 1 diabetes are required for these larger animals. The most common method used for inducing insulin dependence in large models is pancreatectomy. Another common method is the use of STZ. STZ is a chemical that destroys the beta cells. These induced models are used when a large animal is needed for a study.
High-fat feeding is a model that can be used. The use of high-fat feeding in C57BL/6 mice was first described in 1988\. Obesity, hyperinsulinemia, and altered glucose homeostasis can be led to by this diet. This is due to insufficient compensation by the islets. Normal chow is exchanged for a diet with substantially increased calories from fat. This is typically around 58% of energy derived from fat, compared to about 11% in normal chow. The amount of food eaten by the mice should be monitored. This is to ensure that compensation by eating less does not occur. Mice are typically fed this diet for several weeks. The resulting weight gain is associated with insulin resistance and impaired glucose tolerance.
Yes, lean animal models of Type 2 diabetes are also studied. It is known that not all Type 2 diabetes patients are obese. These non-obese models are important for research. Models that have beta cell inadequacy are included in this category. This inadequacy is what ultimately leads to overt Type 2 diabetes in humans. Larger animals have also been utilized in Type 2 diabetes research. The disease in cats, for example, resembles the human condition in several aspects. Characteristics common to humans include development in middle age, association with obesity and insulin resistance, and subsequent beta cell loss.
A variety of animal models for Type 1 and Type 2 diabetes are available. The choice of model will depend on the purpose of the study. These models can be used for pharmacological testing, studies of genetics, and understanding disease mechanisms. For pharmacological testing, the putative mechanism of the drug being tested will be instrumental in the choice. In Type 1 diabetes, the main determinant is whether a model of autoimmunity is required. The timing and predictability of onset also vary. For Type 2 diabetes, the mechanisms underlying the hyperglycaemia must be considered. These can include insulin resistance, beta cell failure, or both.